Abstract
Leprosy is one of the oldest diseases in the world. It is also one of the infectious diseases that the WHO actively works to eliminate. Currently, leprosy cases are decreasing at an average rate of 20% per year. Most common clinical manifestations of leprosy, resulting in organ dysfunction and influencing patients’ daily life, are skin, mucosa, and nervous system lesion. For eliminating leprosy, the best policies are finding cases, treating them, making leprosy diagnosis and treatment available, launching the international cooperation, designing national decentralized campaigns, and decreasing the disability and stigma. With continuing efforts and collaborative activities, leprosy will soon be eliminated.
Introduction
Leprosy, also called Hansen's disease, is one of the most important neglected tropical infectious diseases in the world. For a long time, leprosy has been regarded as a disease related to poverty and poor public health. Most of the leprosy cases now are in countries with relative low income and poor public health conditions. According to the WHO’s report, the estimated cases in 2007 was 224,717; cases are decreasing at an average rate of about 20% per year. The main strategy to control leprosy now is disease elimination, and it has achieved great successes; however, there are a lot of challenges.
Leprosy, caused by the bacteria, Mycobacterium leproae, is a chronic infectious disease with long incubation period to develop the disease. Like other famous mycobacterium species, Mycobacterium tuberculosis, host immunity plays an important role in the disease progress and clinical presentations. The role of cellular immunity decides the severity of clinical manifestation.
Most common clinical manifestations of leprosy, resulting in organ dysfunction and influencing patients’ daily life, are skin, mucosa, and nervous system lesions. Before the cause and transmission of the disease were well understood, patients with Hansen's disease were isolated and abandoned from the society. In Taiwan, leprosy, regarded as a shameful disease, was eliminated for more than 50 years. Patients with leprosy were forced to be isolated from the society and lived in a special community. These people were despised, and their human rights were abolished at that time. Though the disease is not regarded as a stigma anymore, these patients freely came back to the society. People are still afraid that leprosy people will hurt them. For memorizing this dark history, the Taiwanese try to preserve their community as a memorial museum to teach about the newer generation the disease and how a wrong attitude influence these peoples’ lives.
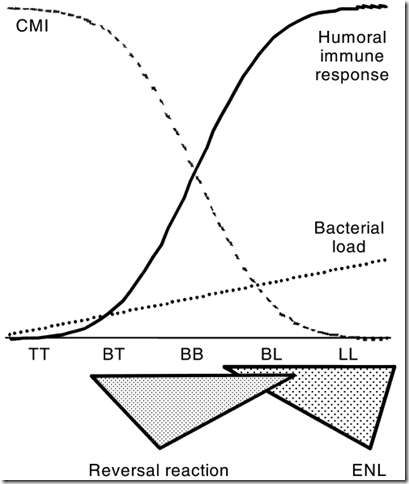
Different host cellular immunity levels have different clinical manifestations. According to the activity of T cells, clinical manifestations in leprosy are divided into five (5-category Ridley-Jopling system): tuberculoid (TT), lepromatous (LL), borderline tuberculoid (BT), midborderline (BB), and borderline lepromatous (BL). The weaker the cellular response to Mycobacterium leprosy is, the more possible the disease presents as the lepromatous type. The stronger the cellular response to Mycobacterium leprosy is, the more possible the disease presents as the tuberculoid type. Borderline types are between them. Another classification for leprosy is based on the amount of bacteria: paucibacillary and multibacillary. The definition is easy to apply; therefore, it is popular in a lot of places.
Schematic representation of the clinical and immunological spectrum of leprosy. CMI, cell-mediated immunity; ENL, erythema nodosum leprosum; TT, tuberculoid leprosy; BT, borderline tuberculoid leprosy; BB, mid-borderline leprosy; BL, borderline lepromatous leprosy; LL, lepromatous leprosy.
left: tuberculoid leprosy middle:borderline tuberculoid leprosy right:lepromatous leprosy
Clinical Manifestations
The most vulnerable tissues or organs for leprosy are skin, mucosa and peripheral nerves. Leprosy is commonly presented as skin lesions, numbness and loss of sensation. Because the peripheral nerves are involved, patients who lost the sensation are unaware of skin damage, resulting in ulceration and muscle dystrophy and dysfunction.
Skin lesions
Early skin lesions start from hypopigmented skin colors. Initially, histocytes are infiltrated into the lesion, and then chronic inflammation progresses and results in granuloma changes. Different host immune responses have different skin presentations.
Tuberculoid type skin lesions usually have few lesions. Well-defined macular or papular lesions with hypopigmented color changes are the main characteristic of the disease. Tuberculoid type skin lesions usually have granulomas surrounding neurovascular elements but with few acid-fast positive bacilli.
Lepromatous type usually presents with nodular lesions. If skin lesions are untreated, the lesions thicken and present as “leonine facies”. Not like the tuberculoid type skin lesions, a lot of acid-fast positive bacilli are noted under microscope.
Nerve lesions
Mycobacterium leprosy affects sensory, motor, and autonomic function of peripheral nerves. Sensory loss is the earliest stage; with the disease progress, more nerves are involved. The most commonly involved nerves are posterior tibital nerve, ulnar, median, lateral politeal, and facial nerves. The nerve damage varies from reduced sensation, loss of sweating, a glove and stocking hypohidrosis to complete nerve loss. Nerves are damaged and dysfunction because of the granulomatous infiltrations. Patients with damaged sensory nerves are vulnerable to the trauma and secondary infections. Like diabetes patients, these people are not aware of dangers around them. However, motor and autonomic nerve damage leads to muscle dystrophy and organ dysfunction, which have great impacts on patients’ daily lives.
Ocular lesions
Blindness is one of the most severe consequences of leprosy. Bacteria either directly infiltrate into the ocular structures or damage the nerve by causing chronic inflammation; with the disease progress, blindness caused by leprosy results in huge disabilities and social economic impacts.
Diagnosis and Treatment
The diagnosis of leprosy needs both clinical suspensions and laboratory diagnosis. Treatments of leprosy need multiple drug therapy (MDT). In WHO regimens, for paucibacillary lesions: Rifampicin 600 mg or Dapsone 100 mg. These treatments need six month treatment course. For multibacillary, Rifampicin 600 mg + clofazimine 300 mg or Clofazimine 50 mg + dapsone 100 mg. These treatments need at least 12 months. Some severe cases need to extend to 24 months. Because the treatments are long, drug adherence and resistance are important issues.
Global Impacts
After a series of hard works, leprosy cases are decreasing. However, no matter cases with active leprosy or cases receiving treatment, disabilities resulted from leprosy have great social-economic impacts.
Leprosy epidemic countries usually are poor countries. These countries do not have good public health prospects for disease detection, prevention, management and rehabilitation. Infected cases are frequently not able to receive the most optimal treatment. Cases with lifelong effects of nerve damage and consequent disabilities are impossible to get rehabilitation and welfare support in these poor countries. Disabled cases and their families need to face stigmas, community rejection, loss of employment, which increase the economic burden of the society and trigger another vicious cycles.
Leprosy has great economic impacts. In the statistics of Special Program for Research and Training in Tropical Diseases (TDR), the Disability Adjusted Life Years (DALYs) of leprosy are 199 thousands (Male vs Female: 117 vs. 82). However, the cost of the disease elimination and prevention proves to be cost-effective. Global leprosy eliminating programs successfully decrease the active cases in a lot of leprosy endemic countries.
Discussion
Treatment Projects
The most effective method for leprosy is treatment. A multidrug therapy (MDT) based on the combination of the antibiotics dapsone, rifampicin, and clofazimine was introduced in 1982 after dapsone-resistant strains appeared and spread. MDT proved highly efficacious in killing the bacteria. Some massive international efforts were launched to eradicate leprosy worldwide. In 1991, the World Health Assembly adopted the target of “elimination of leprosy as a public health problem by the year 2000” Elimination was defined as a reduction in the prevalence of patients with leprosy receiving antimicrobial therapy at a given time to less than 1 per 10,000 populations. This project had successfully cured 13 to 14 million people by MDT1, and full control of the disease (as assessed by prevalence rate) has been officially achieved in 112 of the 122 countries where leprosy was endemic in 1985.
The WHO then started a project2 “the final push to eliminate leprosy”. This final push for eliminating leprosy involves: Making leprosy diagnosis and treatment available, free of charge, at all health centers, particularly in endemic areas; enabling every health worker to diagnose and treat leprosy; dispelling the fear of leprosy, improving awareness of its early signs, and motivating people to seek treatment; ensuring all leprosy patients are cured. These projects successfully decrease leprosy cases in the world. During the past five years, the global number of new cases detected has continued to decrease dramatically, at an average rate of nearly 20% per year.
Through the international cooperation, WHO, World Bank, UNICEF and UNDP launched the TDR projects to eliminate leprosy. WHO also provided free MDT drugs to those endemic countries. In local levels, there are a lot of works needs to do.
National decentralized campaigns
Most of the cases now are in the rural or poor health infrastructures areas1, 3-5. Decreasing the cases in these areas needs to integrate the existing local health infrastructure, public health care workers. Sustaining political commitments are also important. Politicians need to enhance advocacy efforts to reduce the stigma and discrimination against persons and families affected by leprosy. Cases surveillance and registry systems also need to setup to evaluating and monitoring the efficiency of the projects.
Prevention
Although the efficiency of BCG to prevent tuberculosis is controversial, the efficiency of BCG to prevent leprosy has been proved 6. BCG gives variable protective efficacy against leprosy in different countries, ranging from 34% to 80%. Therefore, in leprosy endemic countries, BCG vaccination for children can decrease the incidence of leprosy.
Contacting leprosy patients is a risk factor for the disease, and chemoprophylaxis of close contacts of leprosy patients can be an effective control strategy. In countries with rare cases or chemoprophylaxis are not eligible, health care workers should educate clinical signs of leprosy and advise to report any new skin lesions and contact history to their physicians. Early diagnosis and treatment are the best policies to decrease the disability.
Decrease the Disability
Besides early diagnosis and treatment, adequately protecting damaged nerve and skin tissues are important as well. Educating cases cautiously care their skin. Just as the care of diabetic foots, cases should be taught to wear adequate shoes or gloves when they expose dangerous environment. Any new wounds which are located in denerved regions should adequately clean and care6, 7. For eyes, using tear substitute and antibiotics ointments to protect dry cornea, wearing glasses, and covering with pads are methods to prevent further disability.
Decrease Stigmas
Decreasing stigmas for leprosy is the most difficult mission. However, the best method to decreasing the stigma is curing leprosy. People isolated leprosy cases from the society because they worried about they were infected by leprosy cases. If leprosy can be cured, the stigma vanishes. Public health practitioners, health care workers, and school teachers should teach communities concepts of leprosy transmission, clinical signs and symptoms, and outcome of the treatment. The more people understand the disease, the fewer stigmas will have. Politicians and public figures also should tell the public correct concepts and attitudes for leprosy2, 5, 6; government should legislate to protect these cases’ human right; employers and schools need to accept cured cases to work and study. Only active attitude can decrease the stigma.
Conclusion
With the international cooperation, leprosy cases decreased dramatically. With continuing efforts and collaborative activities, leprosy will be soon eliminated.
Reference
1. Rinaldi A. The global campaign to eliminate leprosy. PLoS Med 2005;2:e341.
2. WHO. Guide to Eliminate Leprosy as a Public Health Problem
Geneva; 2007.
3. WHO regional strategy for sustaining leprosy services and further reducing the burden of leprosy, 2006-2010. Indian J Lepr 2006;78:33-47.
4. WHO global strategy for further reducing the leprosy burden and sustaining leprosy control activities (Plan period: 2006-2010). Indian J Lepr 2006;78:7-31.
5. WHO. WHO Global Strategy Report 2006-2010. Geneva; 2007.
6. Britton WJ, Lockwood DN. Leprosy. Lancet 2004;363:1209-19.
7. Walker SL, Lockwood DN. Leprosy. Clin Dermatol 2007;25:165-72.
繼續閱讀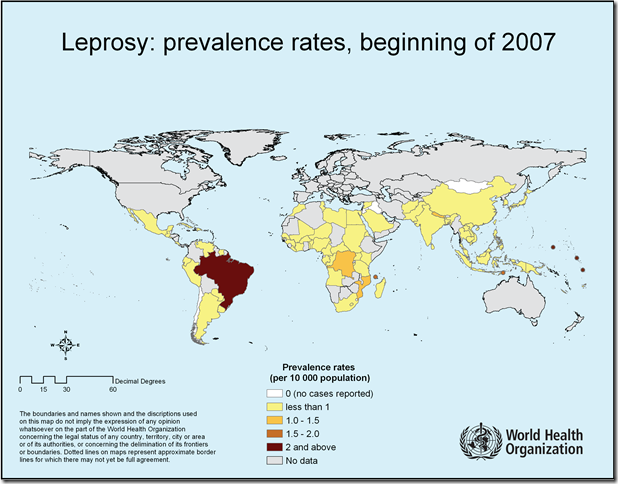








0 意見:
張貼留言